- For Print
- November 5, 2015
Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, “Eisai”) announced today that it has entered into two joint research agreements for the development of new antimalarial medicines.
The first of these agreements is a joint development program with the Liverpool School of Tropical Medicine (Location: Liverpool, U.K.) and the University of Liverpool (Location: Liverpool, U.K.). Under this agreement, the three parties will conduct preclinical development of a new antimalarial candidate compound E209. Research so far has shown that E209 is rapidly acting and shows efficacy against all types of malaria parasites, which means that it could be effective in patients for whom artemisinin-based malaria treatments are ineffective due to resistance.
The second agreement is a joint development program with the non-profit public-private product development partnership Medicines for Malaria Venture (Location: Geneva, Switzerland, “MMV”). Under this agreement, Eisai and MMV aim to ultimately identify antimalarial candidate compounds with novel mechanisms of action that will be effective against malaria parasites resistant to existing treatments, as well as prevent relapse and block transmission to mosquitoes. This involves the optimization of compounds developed by Eisai that inhibit the biosynthesis of glycosylphosphatidylinositol (GPI) necessary for the growth of malaria parasites, and of a hit series of compounds identified from Eisai's compound library through joint research with MMV.
Malaria is a deadly disease caused by malaria parasites that are transmitted to people through the bite of an infected mosquito. According to the World Health Organization1, in 2013 alone, the disease infected approximately 198 million people and led to an estimated 580,000 deaths, mostly among African children. Currently, treatment for malaria combines rapidly-acting artemisinins with lumefantrine and other antimalarials for durability. However, in recent years, there have been reports of strains of malaria resistant to artemisinin. Therefore, the highest priority for researchers is to develop a Single Exposure Radical Cure and Prophylaxis (SERCaP), a single dose drug that would cure patients after one exposure and provide substantial post-treatment protection from relapse as well as block transmission to mosquitoes.
Each of these unique projects was awarded a grant after review by the Global Health Innovative Technology Fund (GHIT Fund), an international non-profit organization that aims to promote the discovery of new health technologies for eliminating infectious diseases prevalent in developing world.
Under its human health care (hhc) philosophy, Eisai is determined to be proactive in improving access to medicines worldwide through partnerships with governments, international organizations, and other non-profit private-sector organizations. Eisai is also actively engaged in several other research collaborations with Brazil's national research agency Fundação Oswaldo Cruz, St. Jude's Children's Research Hospital / MMV, and the Broad Institute to discover and develop new medicines for the treatment of malaria. Through these collaborations, Eisai aims to make new treatments available as early as possible to patients with malaria and thereby further increase the healthcare benefits provided to the patients and their families.
<Notes to editors>
1. About the Liverpool School of Tropical Medicine
The Liverpool School of Tropical Medicine (LSTM) is a non-profit charitable institution with a mission to develop new medicines and vaccines for the control and treatment of tropical diseases, as well as train the next generation of healthcare professionals and researchers. Through collaborative research with LSTM and University of Liverpool (UoL), Eisai aims to identify and develop novel drug candidates that efficiently eliminate the bacteria Wolbachia which live inside, and are necessary for the growth and breeding of, parasitic filariae worms that cause lymphatic filariasis and onchocerciasis (river blindness). In addition, Eisai is conducting preclinical studies in collaboration with LSTM and UoL on candidate compounds for a novel antimalarial treatment that may be effective in patients for whom artemisinin-based malaria treatments are ineffective due to resistance.
2. About the University of Liverpool
The University of Liverpool (UoL) has made major contributions toward the discovery of several classes of anti-parasitic drugs. Over their 20 years in partnership, UoL and LSTM have adopted a “molecule to man” strategy to instigating their research projects, operating at all stages of the drug discovery pipeline up to and including clinical trials in humans. A number of these projects are under progress as joint development projects with the Medicines for Malaria Venture, an organization that has developed many antimalarial drugs.
3. About Medicines for Malaria Venture
Medicines for Malaria Venture (MMV) is a leading non-profit public–private product development partnership in the field of malaria, aiming to reduce the burden of malaria in disease-endemic countries by discovering, developing and facilitating delivery of new, effective and affordable antimalarial medicines. It has the world's largest portfolio of antimalarial medicines in development. Eisai and MMV are also engaged in other collaborations to discover and develop new medicines for the treatment of malaria. For further information, please visit: www.mmv.org/
4. About E209
E209 was discovered through joint research by UoL and LSTM and is a novel tetraoxane-based second generation antimalarial candidate compound. Research so far has shown that it is rapidly acting and shows efficacy against all types of malaria parasites, which means that it could be effective in patients for whom artemisinin-based malaria treatments are ineffective due to resistance.
5. About Glycosylphosphatidylinositol (GPI) Biosynthesis Inhibition
GPI is known to play a key role in the growth and infectivity of malaria parasites. The cell surface of malaria parasites are covered with GPI-anchored proteins that are attached to the cell membrane via GPI, and one of these GPI-anchored proteins called Merozoite Surface Protein 1 (MSP1), is essential for the growth of malaria parasites. By inhibiting the biosynthesis of GPI, essential MSP1 is unable to be anchored to cell membranes; therefore a compound that can selectively inhibit the biosynthesis of GPI has the potential to be developed as a very effective anti-malarial drug. Eisai has selected a group of seed compounds that inhibit the GWT1 protein (an enzyme which catalyzes inositol-acylation) which is essential for the GPI biosynthesis.
6. About the Global Health Innovative Technology Fund
The first of its kind in Japan, the GHIT Fund is a public-private partnership between six Japanese pharmaceutical companies, the Japanese Government and the Bill & Melinda Gates Foundation. Launched in April 2013 with an initial commitment of more than US$100 million, the organization taps Japanese research and development (R&D) to fight neglected diseases. The GHIT Fund invests and manages a portfolio of development partnerships aimed at neglected diseases that afflict the world's poorest people. GHIT mobilizes Japanese pharmaceutical companies and academic and research organizations to engage in the effort to get new medicines and vaccines to people who need them most, with Japan quickly becoming a game-changer in global health. For further information, please visit: www.ghitfund.org
7. About Malaria
Malaria is a deadly disease caused by malaria parasites that are transmitted to people through the bite of an infected mosquito. According to the World Health Organization1, in 2013 alone, the disease infected approximately 198 million people and led to an estimated 580,000 deaths, mostly among African children. Currently, treatment for malaria combines rapidly-acting artemisinins with lumefantrine, amodiaquine, mefloquine and other antimalarials for durability. Artemisinins have been effective against malaria strains that have developed resistance to many of the existing antimalarials used for many years such as chloroquine. However in recent years, there have been reports of strains of malaria having resistance to artemisinin as well. Therefore the highest priority for researchers is to develop Single Exposure Radical Cure and Prophylaxis (SERCaP), a single-dose drug that would cure patients after one exposure and provide substantial post-treatment protection from relapse as well as block transmission to mosquitoes.
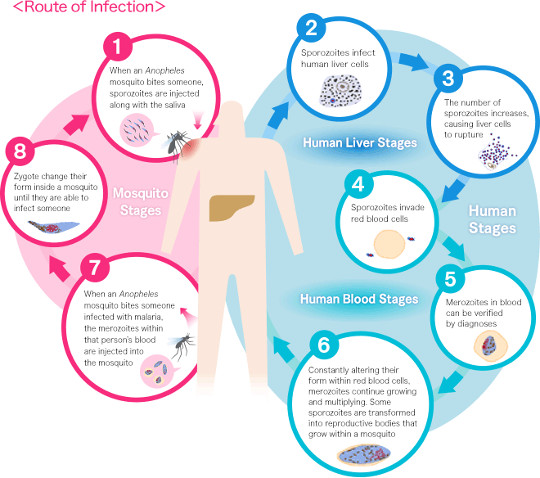
As shown in the diagram, when a mosquito takes blood from a human, malaria parasites in sporozoite form that are injected with the saliva of the mosquito (1) grow in the person's liver cells (2) before then migrating to the blood stream (3) and multiplying within red blood cells (4). This causes the red blood cells to rupture and the parasites to continue invading more red blood cells in a continuous cycle (4 - 6). The symptoms of malaria occur during this cycle, when the parasites have invaded the blood cells, and malaria treatment involves the use of medicines to work on the parasites at this stage. However, it is known that certain species of malaria such as Plasmodium vivax lie dormant in the liver cells instead of growing, and after parasites in the bloodstream (4 - 6) are killed, these hidden parasites in the liver cells awaken later through some kind of stimulus and go on to reproduce and invade the bloodstream again, a process known as relapse.
In addition, most malaria parasites produced in red blood cells (merozoites) are asexual, and will die inside a mosquito if taken during feeding. However, some of these (6) develop within red blood cells into male and female gametocytes that can reproduce inside mosquitoes (7 - 8), which leads to malaria transmission. As such, if these male and female gametocytes can be killed while in the bloodstream of humans, it is possible to block the transmission of malaria to mosquitoes.
- 1World Health Organization: http://www.who.int/mediacentre/factsheets/fs094/en
